The government turns a blind eye to the sale and purchase of sensitive medicines through online pharmacies, prompting the possibility of a large-scale medical crisis.
Kamala Gurung |CIJ, Nepal
Krishna Acharya, a resident of Anamnagar in Kathmandu, ordered four antibiotic medicines from Hamro Pharma, an online pharmacy. The medicines–Clavam, Ofloxacin, Levofloxacin, and Azithromycin–were delivered to his address shortly after he ordered them.
He did not face any questions from Hamro Pharma while ordering and receiving the medicines. Nor was any doctor’s prescription required. The four antibiotics Acharya received through a home delivery service cannot be taken without a doctor’s prescription and advice.
According to Article 17 (2) of the Drugs Act 2035) 1979), “No person shall sell or distribute such drugs without prescription of a doctor as categorized not to be sold or distributed without such prescription according to Sub-section (1). The pharmacist or pharmacy assistant or professional person himself shall sell or distribute such drugs on prescription of a doctor; and the presence of a pharmacist or pharmacy assistant or professional person shall be compulsory where a person other than the doctor, pharmacy assistant or professional person sells or distributes such drugs.” This means that it is illegal to sell medicines without a prescription if they are classified to be sold only with a doctor’s prescription. However, in clear violation of the legal provision, Hamro Pharma delivered the antibiotics without asking a question or requiring a doctor’s prescription.
Lately, social media has been abuzz with advertisements of online pharmacies offering various discounts and services on the online delivery of medicines. We observed the modus operandi of one such pharmacy through Krishna Acharya, a social media user. We wanted to understand how medicines were delivered online and if the service providers required any doctor’s prescription from the consumers.
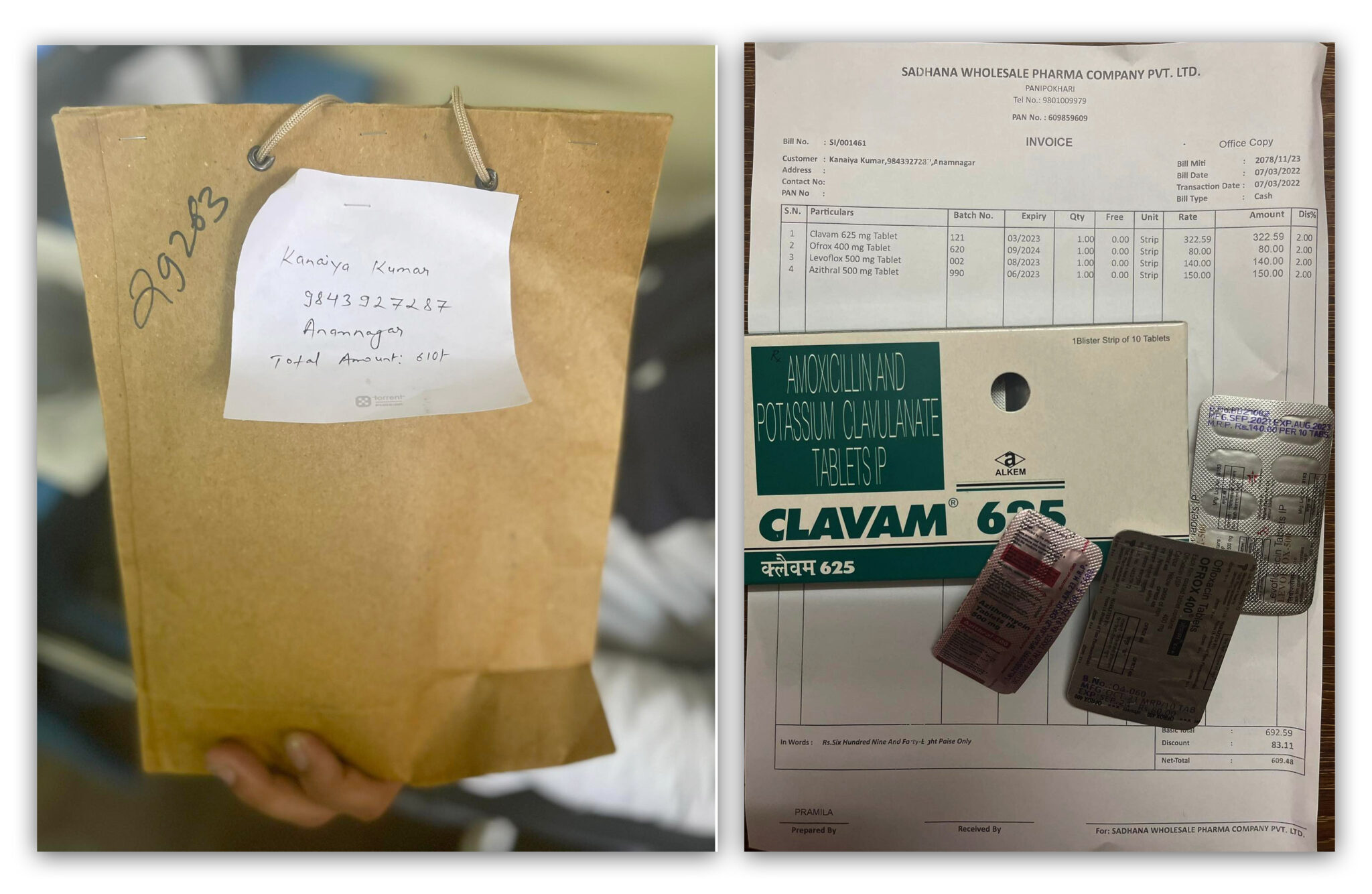
Medicines ordered by Krishna Acharya from our Pharma online pharmacy. Photo: Krishna Acharya
We got our answer when Hamro Pharma delivered the medicines without questions or prescriptions. But we wanted to understand if the violation of the Medicine Act was a one-off incident or a widespread problem. We found our answers when Hamro Pharma delivered the medicines we had ordered. But we were curious to understand whether it was an exceptional case of a common practice. A simple search on social media showed many online pharmacies, including Medi Nepal, Chemist Nepal, GV Nepal and others. When we ordered Amoxicillin and Azithromycin from Medi Nepal, it delivered the antibiotics quickly. They did not ask for a doctor’s prescription. Nor did it ask any questions related to health and illness.
Consuming medicine without proper consultation with doctors runs the risk of taking lives or causing long-term hazards, even if the medicines thus consumed are otherwise life-saving. However, the lack of regulation means that the medicines that are strictly sold on the basis of a prescription are being sold openly over the counter.
To understand more about such transactions, we contacted ‘Hamro Pharma’, where we had initially bought the medicines from. “You did not even ask for a prescription when we ordered antibiotic medicines from your pharmacy. Isn’t it necessary?” Upon hearing this question, the staff initially hesitated, then claimed that the medicines were delivered only against the furnishing of a prescription. He added, “However, we do not ask for a prescription from patients who purchase medicines regularly from Hamro Pharma.”
Contrary to Hamro Pharma staff member’s claims, Krishna Acharya had bought medicines from Hamro Pharma for the first time. He was not asked to produce a prescription. When we asked the staff to provide us with the name and telephone number of the operator of Hamro Pharmacy, he refused to do so.
Department of Drug Administration clueless
When we tried to find out about the legal framework to regulate the online sale and purchase of medicines, we found another interesting fact. In Nepal, medicine transactions are regulated under the ‘Drug Act 2035’. The government has classified medicines into groups (A, B, C & D) per their usage. Based on the Drug Act 2035 (1978) and the Drugs Category Rules 2043 (1986), the classification clearly states which medicines need a prescription for sale and purchase.
However, the Act does not have any provision related to selling and purchasing medicine through online pharmacies. Sub-section 1 of Section 19 says, ‘No person shall make false or baseless claims or advertisements about the usage, utility and efficacy of medicines.’
As per the Act, the responsibility of assessing whether pharmacies operate legally falls on the Department of Drug Administration. However, the department has no idea about online pharmacies. It has no idea how many online pharmacies operate and how they function and sell medicines. Nor does it know the type and quantity of medicines sold through online pharmacies.
Why is this happening? According to Santosh KC, information officer and drug administrator of the department, “The department has not given anyone any authority to operate online pharmacies since there is no such provision in the Act. That is why the department does not have any information about how online pharmacies are under operation and how they are operating. If somebody is operating such pharmacies, it is illegal.”
Isn’t it the department’s responsibility to regulate such pharmacies if they are operating illegally? When CIJ asked KC this question, he responded, “We have no idea how to do it because there is no such legal provision. Maybe something will happen if the Drug Act is revised.”
Bharat Mani Bhattarai, director-general of the Department of Drug Administration, is aware that online pharmacies are illegal. He also concedes that there are unlawful practices even within the pharmacy profession and not just online pharmacies.
“We even published a notice saying that the online sale of medicines was illegal. We are still thinking about what to do with them,” Bhattarai said. “The law says that a pharmacy should be physically existent. Online pharmacies are an unfair practice.”
But the department has no plans to regulate online pharmacies.
Bhattarai said the legal provision to regulate online pharmacies had yet to be brought in due to the lack of budget and other issues. Even as the department washes its hands off the responsibilities to regulate online pharmacies, the Ministry of Health and Population says it is the department’s responsibility to regulate online pharmacies. According to Dr Sameer Kumar Adhikari, joint spokesperson of the ministry, the department should regulate online pharmacies as per the Drugs Act and Guidelines. The ministry, which considers online pharmacies illegal, has no plans to regulate and control them.
“There is no doubt that online pharmacies are illegal because there is no law to address them. We are planning to consult with experts on how to move ahead. For now, let’s say it is illegal.” said Dr Adhikari.
Irregularities galore in medical shops; online pharmacies could be worse.
On March 11, 2021, the Nepal Pharmacy Council visited pharmacies and advised pharmacy operators to wear a white apron, clearly displaying their name tags, while selling medicines. While asking operators to stop misusing the names and certificates provided to operate pharmacies, Sanjeev Kumar Pandeya, the council’s registrar, visited places such as Banasthali, New Bus Park, Gongabu and Jawalakhel. During these visits, he saw many irregularities in the pharmacies.
Out of the 34 pharmacies the council team visited that day, 14 had flouted the law as unauthorised persons were running them, and three were being run without permission. So much so that individuals who had no idea about medicines were found selling medicines that a pharmacist could only sell. Some were even running medical shops by ‘renting’ the licences of others.

According to Pandeya, such a situation can be found in medical shops on each street corner of the city. One reason for this is the debate regarding whether the pharmacy proprietor and the medicine reseller need to be the same person or not.
As per the Act, only a pharmacist or assistant pharmacist under the pharmacist’s supervision can sell medicines. Such pharmacists and assistant pharmacists must be registered with the Nepal Pharmacy Council.
The Nepal Pharmacy Council Regulation 2059 (2002) considers pharmacists and assistant pharmacists as pharmacy proprietors. According to this provision. There is no contestation of the fact that the pharmacist and assistant pharmacist are the ones that are the pharmacy proprietors. However, a decision by the department has messed up this provision.
Article 17 (2) of the Drug Act, 2035 says, “While selling medicine on the basis of the doctor’s prescription, the pharmacist or the assistant pharmacist should do so. When others are selling the medicine, they should do so in the presence of the pharmacist or the assistant pharmacist.” While interpreting this provision, the department, on November 3, 2014, decided that the pharmacy proprietor and the trader could be different. On this basis, anyone can run a pharmacy in collaboration with the pharmacist.
This provision has resulted in chaos, which is evident in the department’s statistics. While 79 pharmacies of 10 districts were penalised in the fiscal year 2020/21, 113 pharmacies of 9 districts were punished in 2021/22. Of the 79 pharmacies that faced penalty in 2020/21, 68 were run by others than the authorised persons. In 2021/22, there were 89 such pharmacies of the 113 that faced the penalty.
According to Pandeya, the council’s registrar, “If the pharmacist or assistant pharmacist is the proprietor, they are likely to care for public health. They are aware of the effects of medicines, and there is little chance of misuse. We do not say that only the proprietors can sell the medicines. But when they are absent, they should get a pharmacist to sell the medicines.”
If formally registered pharmacies are operating with such negligence, it would not be a surprise if online pharmacies are operating under total chaos. Pandeya says medicines cannot be sold online as they risk taking lives. “A patient’s health might deteriorate or even die if some medicines are taken without a doctor’s advice. This cannot be taken lightly. If the Department of Drug Administration does not take concrete action, it will be difficult to control the menace caused by online pharmacies.”
Local government clueless
It is the Department of Drugs’ direct responsibility to check whether pharmacies are operating as per the law and to penalise them if they are going against it. Lately, local governments are constitutionally endowed with authority regarding health and education. They are responsible for its monitoring and regulation. What is the local government doing regarding this?
We tried to understand what Kathmandu Metropolitan City was doing in this regard. But the metropolitan cannot regulate the pharmacies established in their area. The metro city was found unable to control online pharmacies under its jurisdiction. Bala Ram Tripathi, the chief of the Department of Health at Kathmandu Metropolitan City, said, “Online pharmacy is a new issue for us. We will now try to understand what it is.” Tripathi further said the metropolitan city would now start keeping health institutions’ records and discussing what to do with online pharmacies. “If it is illegal, we have to control them; if necessary, we have to regulate them judiciously. We do not have any such plan now, but since it is related to public health, we need to take it forward,” Tripathi said.

Kathmandu Metropolitan City is not the only local-level government that fails to consider it a problem. Kala Nidhi Devkota, an executive director of the Nepal Federation of Municipalities, said no local government had made any plans regarding online pharmacies. “The federal government should first make guidelines or laws. Local governments can then implement and monitor the online pharmacies based on those guidelines or laws.”
Online and e-pharmacies are in operation in many countries. Those countries are making online pharmacies more secure and are implementing laws related to the same. According to Dr Lochan Karki, chairperson of the Nepal Doctors Association, online pharmacies that the government has not authorised should be regulated by formulating a law.
If the existing pharmacies are not regulated properly, is it possible to regulate online pharmacies? Dr Karki does not have an answer. “If you and I visit a pharmacy nearby and ask for an antibiotic, will they give us one or not? How can the regulatory bodies regulate online pharmacies if we cannot regulate the existing pharmacies?”
According to Dr Karki, patients who visit him come only after taking antibiotics on their own. “Many patients come to me after they fail to get better after taking Azithromycin for fever, headache or other ailments. Some of them even receive an injection at the pharmacies. It is necessary to check the status of the lungs and kidney function of the patients while administering various medicines. However, patients take such medicines unscrupulously and risk their lives, and the blame goes to the doctors.”
Globally, one of the biggest health challenges is resistance to antibiotics. If antibiotics can be bought easily, like in Nepal today, it will lead to a situation where antibiotics won’t work against infections. According to Karki, “We have limited kinds of antibiotics. It takes a long time to create a single antibiotic medicine. If the existing antibiotics are misused and made ineffective, what antibiotics will we give in serious cases?”
This malpractice continues due to the weakness of the Department of Drug Administration, the regulatory body, says Dr Sharad Onta, a public health expert. “If the department becomes efficient, even local levels can monitor the sale and purchase of medicines under the department’s guidance. But for that, even the local levels need structures that help complete this task,” Dr Onta told CIJ Nepal.
Online pharmacies are a challenge to public health: Dr Onta

Dr Onta. Photo: Swasthya Khabar
Medicines directly related to human health are not ordinary objects that can be home delivered through online services. If medicines are sold and purchased through online pharmacies, there is a risk of the medicines being misused. This is a serious issue from the viewpoint of public health. Misuse of medicines causes multi-dimensional adverse problems. Antibiotics stop working if medicines that cannot be sold without a doctor’s prescription are sold freely.
I have heard there are plenty of online pharmacies in the city these days. Why is an online pharmacy needed when there are brick-and-mortar pharmacies everywhere? Online pharmacies might rather have a utility in rural areas where medicines are not readily available. But even for this, the government should develop and implement laws, regulations and guidelines related to the issue.
Online pharmacies are established for business rather than for the service of patients. When the government fails to regulate and manage physical pharmacies, the mushrooming of online pharmacies leads to chaos.
Medicines that cannot be sold without a doctor’s prescription
According to the Drug Act, 2035 and the Drugs Category Rules, 2043, the medicines divided into ‘Group A’ include those related to narcotics and poison; ‘Group B’ consists of antibiotics and hormones, etc. The drugs in these categories should be sold with a doctor’s prescription. Similarly, only pharmacists or proprietors should sell these medicines in the presence of either a pharmacist or a proprietor.
‘Group C’ medicines can be sold without a prescription based on experience. There is no need for a pharmacist’s or proprietor’s presence while selling them.