Basanta Pratap Singh in Bajhang; Krishna Adhikari in Nepalgunj; and Laxmi Basnet and Bidya Rai in Kathmandu: Centre for Investigative Journalism-Nepal
On June 21, a 30-year-old man died by suicide at a quarantine centre in Pathibhera Rural Municipality-7 in Sudurpaschim Province’s Bajhang District. He had returned from India three days earlier and was being quarantined along with fellow returnees Umesh Bohara and Janak Bohara.
“He’d often say he wanted to lock his room from the outside and head home. He didn’t speak with anyone one day,” said Umesh. “He hanged himself the following day. We came to know about the incident only in the morning.”
The quarantine was ill-managed and failed to meet the minimum standards for the safety and wellbeing of the inmates. There was no one to counsel the anxious youth who had returned home. And the centre didn’t provide even basic amenities such as food and decent lodging. “No one came to check up on how things were at the quarantine because of the fear of coronavirus transmission,” said Janak. “The police came once in three or four days, inspected the quarantine from afar, and went back.”
Suicide zones
The list of people dying by suicide–inside quarantines and in the society at large–owing to coronavirus-induced anxiety is getting longer. On July 3, an 18-year-old youth from Bajhang’s Khaptad Chhanna Rural Municipality hanged himself upon being informed that he had tested positive for the virus. He had returned from India in a group of 16 and was quarantined for 14 days before being sent home on June 28.
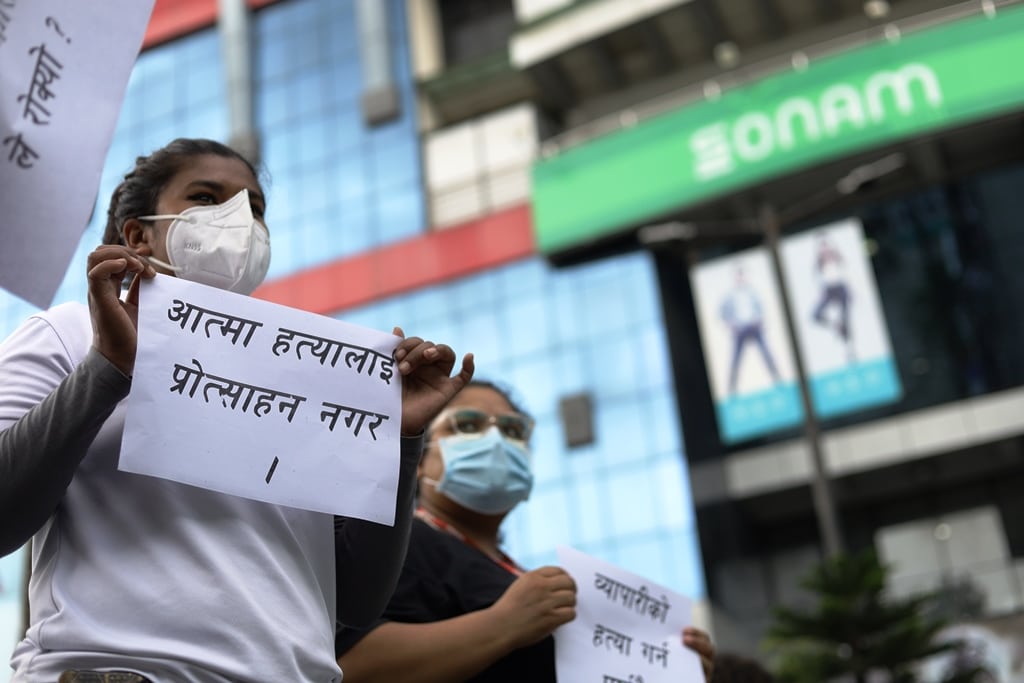
A shop owner outside Civil Mall holding a sign that says “Do not encourage us to commit suicide.” All shops had been closed owing to lockdown but shop owners were forced to pay rent. Photo: Subhash Shresha
“He was last seen herding buffalo in a jungle nearby,”said Ram Bahadur Singh, spokesperson of the rural municipality. “In the meantime, someone called to inform him that he had tested positive. He was later found hanging from a tree.”
On June 13, a 45-year-old man who was quarantined at Satyavadi Secondary School in Bajura’s Badimalika Municipality-2 died by suicide. He had returned from India two days earlier and had tested positive for the virus on June 14.
Others who died by suicide while being quarantined include a 45-year-old man from Arghakhanchi’s Sitganga-5; a 31-year-old man from Rolpa’s Gangadev Rural Municipality-5; and a 49-year-old man from Tanahun’s Ghiring Rural Municipality-3. All three of them had returned from abroad and were in quarantine when they tested positive for the virus and couldn’t bear the stress after knowing about their condition.
As per the Nepal Police Headquarters, 11 individuals died by suicide while being quarantined in the two-month duration between May 1 and July 9 .
“Among those who committed suicide, 10 were men and one a woman. All but three of them had tested positive for coronavirus,” said Niraj Bahadur Shahi, deputy inspector-general and spokesperson of the Nepal Police.
Mental health activist Jagannath Lamichhane said the people might have taken their lives because of the stigma they’d have to face owing to their Covid infection. “So many Nepalis take loans to go abroad. And when they find they have been infected with coronavirus, they’re likely to take any step because they can’t deal with the added stress. This problem can’t be solved through medical care alone.”
Sub-standard quarantines
The “Coronavirus Quarantines Operation and Management Guideline, 2076 (2020)”, prepared by the Nepal Government, requires all quarantines to be equipped with primary aid kits, clean and safe bedrooms, and beds spaced out at a safe distance.
The guideline also requires all quarantines to have at least three sanitation workers, enough dustbins, masks, separate soaps and sanitisers, and that the quarantines manage their waste as per the minimum standards prescribed. The guideline also requires medical tests to be conducted on the quarantined twice a day. It also requires the facilities to conduct regular physical exercise and psychological counselling sessions.
However, these amenities and provisions are not available in most quarantines across the country. After their friend committed suicide in the quarantine in Bajhang’s Majhkhori Secondary Schook, Janak Bohara and Umesh Bohara failed to receive any psychological counselling. Unsure of what to do, they invited a local shaman to ward off the evil.
Dr Rupchandra Biswakarma, in-charge at the Bajura District Hospital, said quarantines in Sudurpaschim Province lack the facilities mandated by the guideline. “Furthermore, the local levels have not been able to manage quarantines properly owing to the large number of people coming through them,” said Biswakarma.
The lack of facilities is not limited to Sudurpaschim Province. After monitoring quarantines across the country from mid-March to mid-June, the National Human Rights Commission published a report that said quarantines were found to have flouted the World Health Organisation’s guidelines–which require sufficient food, water and sanitation, implementation of the basic provision for containing transmission, and single rooms, and open space for inmates.
One reason for why the guidelines have been flouted is that most of the quarantines across the country are set up in local schools and community halls. For one, these structures are not designed to house people at night. And they are difficult to convert into spaces for safely housing a large number of people. In many places, including in the Terai, quarantine centres are merely tents erected in fields, under trees. A woman quarantined in Surkhet said she had to sleep on desks and benches, didn’t get any access to electricity for recharging her phone, and had difficulty getting food and a sleeping mattress.
Dr Divya Dawadi, co-spokesperson for the Ministry of Education, Science and Technology, said the school buildings could not meet the guidelines’ requirements and that the manner in which the buildings were repurposed as quarantine centres would not help deter incidents such as rape, theft, and suicide.
“Schools are made for daytime teaching-learning activities, and not for quarantining people,” Dawadi said, adding that such facilities had become unsafe, especially for women and children.
The quarantined, though, say the quarantines’ infrastructure was just one among several shortcomings they had to put up with. They also had to deal with the unhelpful attitude of the managers and volunteers, they said. The treatment meted out to them added to the inmates’ anxiety. They complained that whenever they asked for something, the managers and volunteers would dismiss the requests by telling them they’d already been provided food and lodging.
The quarantines also lack medical testing facilities. And owing to the stress inmates face in the quarantines, mental health experts say the inmates tend to overthink even the smallest health issues affecting them–some tend to excessively worry about a sore throat or cold and cough. Moreover, because many are already burdened with supporting their families despite losing jobs, their stress tends to pile up, with some thus reaching breaking point and resorting to suicide.
“This is evident if we analyse the financial and family backgrounds of those who have committed suicide,” said Dr Narendra Singh Thagunna.
The quarantines are particularly taxing for women, who fear being sexually abused and who have to also have to learn to deal with issues such around menstruation in a new, cramped setting. In Pokhara, a pregnant woman worried that the fetus in her womb had stopped moving for a few days. “I felt better only after I was counselled by a doctor,” said the woman. Mothers who have been quarantined along with young children faced a different problem altogether. The children ask for food time and again. But no food is available except for lunch and dinner.
The Covid testing process itself has led to problems at the quarantines. On June 12, some quarantine inmates blocked the road in Rajpur, Rautahat, for not having received their PCR reports on time (the longer the inmates have to wait for their reports, the longer the time they have to spend inside quarantines). Three policemen were injured while trying to clear the blockade.
In other places, inmates have run away from the quarantines. Inmates ran away from the quarantines in Narainapur, Banke, and Narayan Campus and Bhairav High School, Dailekh, for example. Many such quarantine centres across the country eventually became completely ineffective on account of their large number of inmates.
The inconvenience faced by the Simta Rural Municipality in Surkhet is a case in point. “We did our best to deal with the large number of inmates. We didn’t give up, but we did have about 2,700 people in 48 quarantine centres and one isolation ward in the rural municipality on June 2,” said Kavindra KC, chairperson of the rural municipality.
According to the National Emergency Operation Center, under the Ministry of Home Affairs, 1.38 lakh people were in quarantines in mid-June. Since then, the number has been declining. Of them, 33,737 were women and 4,677 were children. During this period, 267 pregnant women were in quarantine. As of mid-June, 7,110 quarantine centres were in operation across the country.
Psychological counselling is essential
One issue that experts worry about is the lingering after effects of the stress that inmates suffer in qurantines. But there are cases in Surkhet that show that people can return to normalcy with good psychological counselling, no matter how tired, stressed, anxious and angry they might be. Anita, who returned from Mumbai, India, in the third week of May, was quarantined before she could get home. She stayed in a local quarantine with her 11-year-old daughter, who was ill, and two other local boys. She said she was worried that she would not be able to reach home and meet her son, who was in her village.
At the quarantine, Anita faced several problems. The school building had poor ventilation. She had to spend her day sitting outside in the afternoon. The toilet was far away. She was worried about her physical safety when she went to the toilet at night. And she had her youngest daughter by her side. There was no one to talk to or to comfort her. Those who came to see her talked to her briefly from a distance and returned quickly. She felt ostracised, she said.
She would hear reports of people dying from Covid-19 in the country and abroad. Anita said such information added to her stress. “I used to think, ‘What will happen even if I survive?’” In the meantime, her daughter tested positive. Anita too tested positive after a few days. Both were relocated to an isolation centre. After that, Anita said, she began questioning whether it was worth living anymore.
After Anita shared her anguish with her friends, she was referred to Sharmila BC, a psychologist.
“Sharmila spoke with me on the phone for a long time and encouraged me,” said Anita. “More and more people were added to the isolation centre. The time passed quickly as we shared our griefs. Eventually, I won over the coronavirus and returned home after 35 days.” She now counsels other coronavirus patients.
Addressing mental health issues of inmates is of utmost importance, say experts. “Counselling and yoga energise the mind and help reduce the stress of those living in quarantine and isolation centres,” said Bhojraj Sharma, a psychologist based in Nepalgunj. According to Sharma, there are other ways to manage stress, such as avoiding incomplete, unreliable, and inaccurate news doing the rounds on social media, exercising and meditating, getting enough sleep, and talking to friends and loved ones. “This helps inmates find some peace of mind,” said Sharma.
According to PD Saroj Prasad Ojha, Head, Department of Psychiatry, Tribhuvan University Faculty of Medical Studies, the government must seriously address how the quarantine centres are being run.
“Quarantines are not prisons, and basic amenities should be made available to everyone,” he said. “We need to create an environment for maintaining social distancing. We also need to create an environment for sleeping on time, getting up on time, and doing exercise and yoga after waking up. We need to create an environment that promotes engagement in one thing or the other so that the quarantined don’t suffer from loneliness and depression.”
The lockdown’s impact on mental health
As is the case elsewhere around the world, the Covid crisis–especially the lockdown– has taken a toll on Nepalis’ mental health.
“Mental health problems have increased since the lockdown,” said psychologist Bhojraj Sharma. “The economic crisis has caused undue stress among Nepalis. Police say the number of suicides has reached 1,800 in the three months following the lockdown, which is quite alarming.”
The recently lifted lockdown also had an adverse effect on the government’s ability to provide psychosocial care. Before the lockdown, the government and private organizations were running satellite clinics to provide psychological counselling and mental health treatment. But such clinics could not operate properly during the lockdown.
Similarly, owing to the lockdown, medicines could not be provided to mental health patients, through primary health centres, in rural municipalities and municipalities. During the current crisis, only a handful of rural municipalities and municipalities in the country have been able to deliver medicine door-to-door for patients suffering from chronic diseases.
Suresh Dhakal, an anthropologist, said all these problems have resulted from the state’s failure to plan for and provide the requisite services, facilities, and security. “Our old social and cultural security structures crumbled,” said Dhakal. “Subsequently, those who needed social security from the state didn’t get any help. That is why we faced mental health problems on such a large scale.”
Whatever the reasons for the state’s lapses, psychologist Dr Narendra Singh Thagunna said, a mental health literacy and awareness campaign should be started immediately to check the suicide rate and address the mental health crisis. “Access to mental health care should be expanded at the community level,” said Dr Singh. “The existing mental health services should be made effective, and additional helpline services should be made accessible. The government can significantly reduce suicides and psychosocial problems if it, for example, rolls out self-employment and skills promotion programmes targeting migrant worker returnees.”
Apart from governmental efforts, family members also play an important role in keeping their families safe. Experts say family members should be able to identify any abnormal behaviour among family members and help resolve it through communication and personal care. According to Dr Singh, if a person shows signs of being suicidal, the problem should be addressed immediately.



